Mental Health · Physical Health
Sleep may be the secret to good mental health. Do you know how to get what you need? Check out sleep expert Glenn Landry’s article for some tips.


January 11th, 2019
Sleep Matters!
by: Glenn J Landry, PhD
We’ve known for decades the importance sleep plays in growth, repair, and restoration of both the brain and body. Recent advances in neuroscience have provided us greater insight into the mechanisms by which sleep accomplishes these feats. For example, we now know that sleep literally washes our brain of the day’s waste. It turns out the act of being awake is toxic, and that sustained wakefulness beyond 16 hours results in physical and mental impairments equivalent to those observed following alcohol consumption. In fact, impairments due to sustained wakefulness greater than 19 hours are much the same as those observed in individuals who are legally too drunk to drive. A good night’s sleep is the only remedy for wakefulness. The good news is that we only need 8 hours sleep to wash away a 16 hour day!
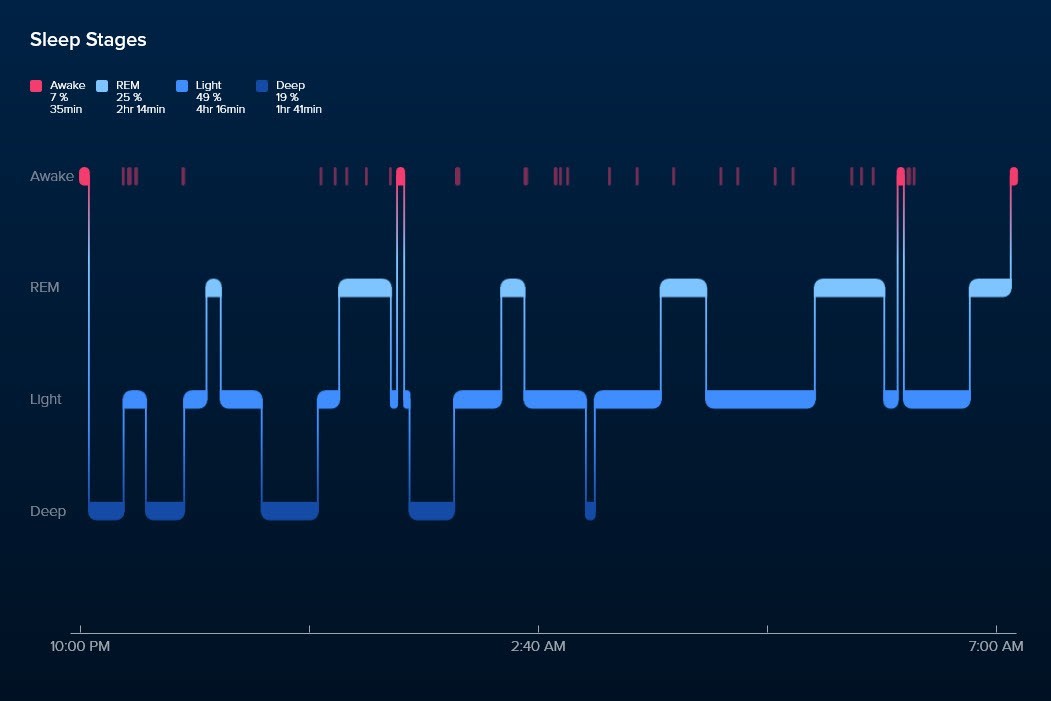
Here’s what elite sleep looks like using Fitbit’s Sleep Stages:
Elite Sleep
Here’s what to look for in elite sleep:
- Rapid entry into Deep sleep, indicating readiness for sleep
- First half of the sleep window (i.e. the time spent trying to sleep) is spent predominantly in Deep sleep, alternating with REM sleep
- Second half of the sleep window is spent alternating between REM and Light sleep
- Awake periods (red bars) are very brief (less than 10 min), accounting for less than 10% of the entire sleep window
- Deep sleep = 90 min (19% of an 8 hour sleep)
- REM sleep = 120 min (25% of an 8 hour sleep)
As I have said many times to anyone who was willing to listen: If we want to be elite in whichever domain we have chosen for ourselves, we must first become elite sleepers!
Sleep Debt & Exhausted Brain
We live in a 24/7 society where sleep is the first thing we sacrifice to meet the growing demands of work, family, and our friends. Sadly, many of us are getting less than 7 hours sleep each night and the timing of our sleep window swings wildly from night to night and week to week. Our hectic schedule makes shift workers of us all, and as a result we subject ourselves to social jetlag. Chronic short duration, opportunistic sleeping patterns are as toxic as a single night of total sleep deprivation, and yet for so many of us, we’ve fooled ourselves into thinking we can get by fine with the little sleep we’ve come to accept as the new normal. But like a fog that rolls in slow and steady – making it difficult to see the hazards ahead – neglecting our need for sleep brings with it a tsunami of health hazards including dementia, obesity, type 2 diabetes, cardiovascular disease, and cancer. The sleep science is definitive now… chronic short-duration sleeps result in a wave of toxicity originating in the prefrontal cortex and rolling through the brain. The scariest sleep science to date is the growing evidence that sleep debt begets more sleep debt. Our capacity to get deep sleep initiates in our frontal cortex and the toxic waste that remains following chronic short sleeps actually decreases our capacity to get the deep restorative sleep we need. These findings help explain the plight of the insomniac who knows all too well they need more sleep, but can’t will themselves to better sleep.
Sleep Debt & Mental Health
The correlation between psychiatric illness and poor sleep has been well documented, but the prevailing wisdom until quite recently was that best practice was to treat the illness using pharmaceuticals and/or therapy… and in doing so, sleep disturbances would remedy themselves.
Fortunately, neuroscience has progressed and we now know a bidirectional relationship exists between sleep and mental health. Chronic short-duration sleep can actually cause or worsen psychiatric illnesses, and now we know why.
In much the same way that sleep debt builds toxicity in the frontal cortex – disrupting the capacity for deep restorative sleep, chronic short-duration sleep disconnects the rational brain (i.e., the prefrontal cortex) from the emotion (i.e., the amygdala) and reward (i.e., the striatum) centers of the brain, thereby disrupting our capacity to manage our emotions and control our appetite for reward. Therefore, care plans designed to address mental illness should include objective sleep assessment – and, when necessary – sleep interventions to promote sleep health. Given the bidirectional relationship between sleep and mental health, best practice would be to promote sleep health in combination with standard treatment of mental illness.
Sleep Debt & the First Responder
With this understanding of sleep’s restorative powers, let’s consider sleep routines and their consequences for the most heroic of shift workers, the First Responder. Countless studies have documented the woeful sleep of shift workers. Perpetual shifting – turning days into nights and nights into days – exposes all shift workers to a growing list of known health hazards. In fact, in 2010, the World Health Organization, after a thorough review of the science, determined that shift work and its resulting impact on clock function does act as a clear carcinogen. If that wasn’t bad enough… the news for First Responders is much worse. Because the nature of their work exposes First Responders to incredible stress and trauma daily, they are in greater need of restorative sleep than anyone. We are just beginning to understand the depths of psychological injury our First Responders endure, often in silence. There is much research to be done in this area, but make no mistake… we already know enough to make a difference now. The current sleep science provides us with the knowledge and tools necessary to help our heroes get the sleep they need. I would argue for those of whom we’ve asked so much, our debt is far greater than gratitude or financial security could repay… we owe them the rest and recovery they so richly deserve.
A Call to Action
If we continue on our current path of longer days and shorter sleeps, in the decades to come we will learn the true cost of sleep lost. For those individuals who smile and say “I’ll sleep when I’m dead”… sleep will come sooner than expected. The years preceding their premature demise will be defined by accelerated diseases of aging. Nations, too, will pay the price… the cost of exponential increases in healthcare utilization, not just for an aging demographic but across all demographics.
It is the dawning of a New Year and my sincere wish is that 2019 marks a change in the way we prioritize sleep in our society. Longer days are not the path in search of ever increasing productivity. Instead we must seek these gains in our dreaming state. It is by sleeping well that we give ourselves our best chance to make the most of our waking day!
Sincerely,
Glenn J Landry, PhD
Sleep Consultant

604 862 9458 | glenn@elitesleep.ca